A New Framework for Digital Diabetes Prevention
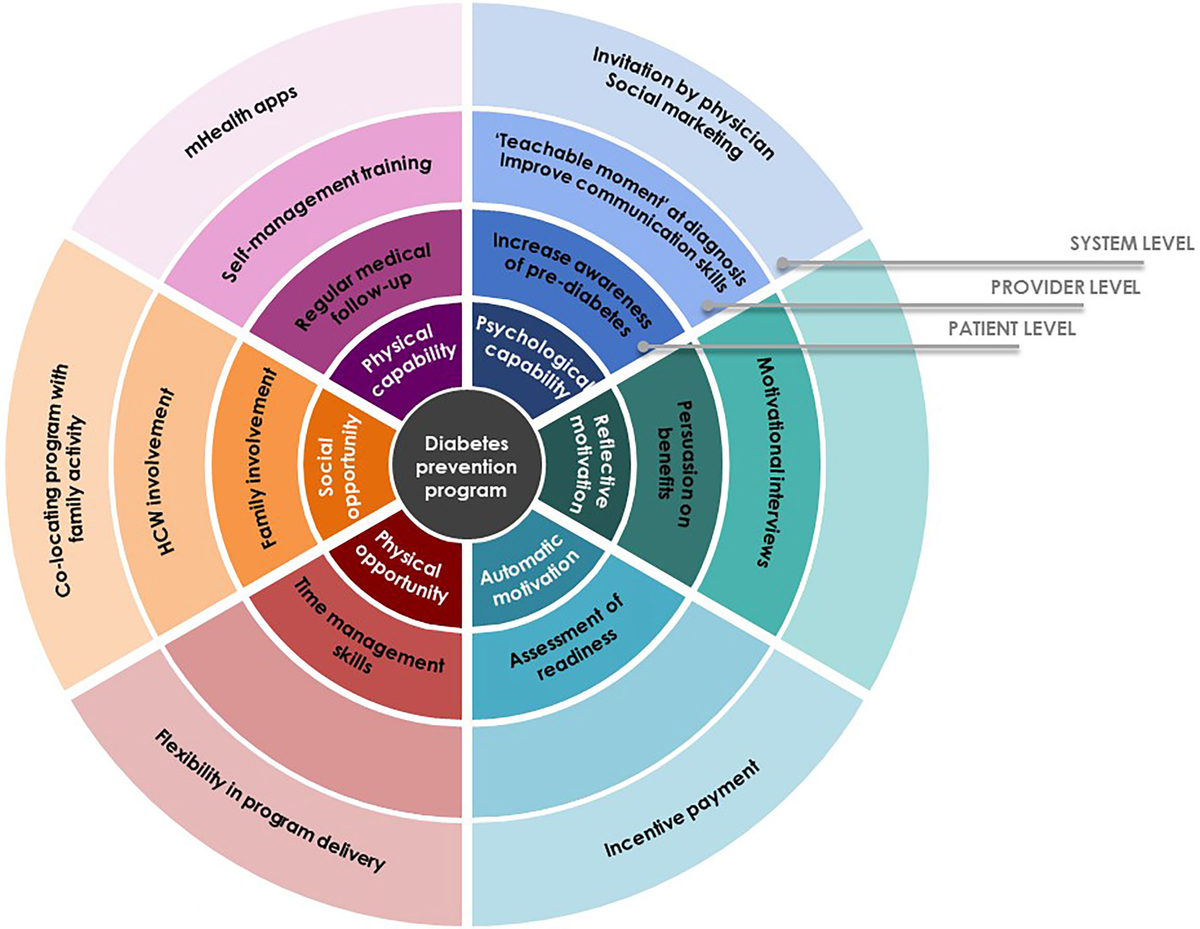
In the age of smart tech and real-time data, health is no longer just about what happens in a doctor’s office. It’s about daily behaviors: how we eat, sleep, and move. This shift from a reactive to a proactive model is changing how we approach chronic conditions like diabetes. Joe Kiani, founder of Masimo and Willow Laboratories, has long championed prevention that fits real life. With Nutu™, his latest innovation, he is helping to modernize early intervention by making it more accessible, more adaptive, and more aligned with how people live today.
It’s time to reimagine programs like the National Diabetes Prevention Program (DPP) not as a fixed curriculum, but as a flexible framework, personalized, tech-enabled, and capable of reaching more people where they are. This means building experiences that feel less like a program and more like a partnership in health, adapting to individual needs without losing clinical integrity.
A Proven Model, Ready for an Update
The traditional DPP focuses on helping participants lose weight, eat better, and increase physical activity through group sessions and coaching. The model has demonstrated clear success in reducing the risk of diabetes for those who complete the program.
Yet the format, often dependent on scheduled sessions, in-person meetings, or static lessons, doesn’t always match the realities of daily life. Participation rates drop, follow-through declines, and access remains uneven across regions and demographics. Digital platforms offer an opportunity to update the delivery model without losing the behavioral science at its core.
Meeting Users in the Moment
A reimagined DPP would make support continuous, not limited to scheduled check-ins. With the use of tools that connect biometric and behavioral data, support can be offered when users need it most. This real-time feedback removes the delay between learning and action, building self-awareness and helping users apply what they learn as they live, not just after a session ends.
A user who skips breakfast and logs poor sleep might get a morning hydration reminder and a prompt to prep an easy meal. Another who shows signs of elevated glucose may receive coaching on adjusting dinner timing. This kind of real-time feedback removes the delay between learning and action. It builds self-awareness and helps users apply what they learn as they live, not just after a session ends.
From One-Size-Fits-All to Adaptive Personalization
The original DPP is built on a structured approach that can feel rigid, especially for users juggling work, caregiving, or inconsistent schedules. A digital-first framework doesn’t just digitize this structure; it makes it personal for the user. Platforms adjust to individual goals, habits, and readiness for change. Instead of prescribing the same actions for everyone, they guide users toward the next best step.
This might mean encouraging more movement after a sedentary day or offering a reminder to de-stress after a rough night of sleep. This behavior change feels realistic because it’s based on the user’s actual behavior, not on a generic program.
Joe Kiani, Masimo founder, notes, “What’s unique about Nutu is that it’s meant to create small changes that will lead to sustainable, lifelong positive results.” That thinking is central to this new approach to health. A digital framework grounded in daily feedback and behavioral design can support the same goals, without overwhelming users. It helps users engage longer, act more often, and build trust in the process.
Expanding Reach Through Technology
One key advantage of a digital DPP is reach. Many people at risk for Type 2 diabetes never join a reduction program, not because they’re not interested, but because access is limited. They may live far from providers, work unpredictable hours, or lack the transportation or time to attend regular sessions.
Digital programs help to lower those barriers. There’s no need to commute, log in at a specific time, or catch up on missed content. That flexibility brings prevention into more homes, jobs, and routines and into communities that need it most.
Supporting Consistency Over Compliance
A common reason people drop out of rehabilitation programs is that they feel too structured or too demanding. Digital platforms can shift the focus away from perfect attendance or completion rates and toward steady progress. If a user misses a check-in or logs a setback, the platform responds with encouragement and a path forward. This approach keeps people engaged without shame or rigidity. It also acknowledges that health is not linear. The reimagined DPP should reflect that, offering support that adjusts to life’s ups and downs.
Connecting the Platform to the Provider
A strong digital program doesn’t isolate users, but it strengthens care relationships. Data collected through platforms can be shared with primary care teams, helping providers understand what’s happening between visits. It creates more informed check-ins, more tailored advice, and a better patient experience. It also helps clinicians intervene earlier if trends shift in the wrong direction. When tech and clinical care work together, the reduction effort becomes more cohesive and more successful.
Making Outcomes Visible
Another benefit of digital-first reduction is visibility. Many people abandon health programs because they don’t see immediate results. But platforms that track biometric signals, like glucose trends, recovery scores, or sleep quality, can show progress users might not otherwise notice. These wins reinforce behavior. When someone sees a dip in resting glucose after consistent morning walks, or improved sleep after changing their meal timing, they’re more likely to continue. That kind of positive reinforcement is essential for long-term success, and it’s a key reason digital tools improve adherence.
Reaching More People with Less Friction
The traditional programs remain effective for those who complete them. But if it’s too difficult to access or sustain, its impact is limited. A reimagined framework, built around real-time guidance and behavior-first design, removes many of those limitations.
It doesn’t replace the core science, but it delivers it differently, with less friction, more flexibility, and tools that understand how people actually live. Nutu reflects this direction to support simple, sustainable and built around the user, not just the protocol.
A Smarter Path Forward
The future of diabetes reduction isn’t a new program, but a smarter framework, one that adapts to individual needs, integrates with digital routines, and turns goals into daily action. By expanding on the DPP’s foundations and applying them through intelligent platforms, we have an opportunity to reach more people, keep them engaged longer, and help them confidently prevent chronic conditions. When reduction is personal, consistent and easy to access, more people succeed. That’s the future the DPP was always meant to serve.